Most people don’t realize this, but vitamin D isn’t actually a vitamin — it’s a hormone your body makes from sunlight. That one fact changes everything.
We’ve been told to take vitamin D pills through winter and trust that they’ll do the same job as the sun. Yet despite record supplement use, deficiency rates keep rising. Something isn’t adding up.
This article breaks down the real science behind vitamin D — what it is, why it matters, and how to get it the way nature intended. You’ll learn how vitamin D from sunlight, food, and supplements each affect the body differently, why modern life has disrupted this balance, and how to restore it safely.
What Vitamin D Actually Is (and Isn’t)
One of the biggest misconceptions about vitamin D is that it isn’t really a vitamin at all. It’s a prohormone — a raw ingredient your body turns into a powerful hormone that regulates immunity, metabolism, and calcium balance.
It also doesn’t really behave like a vitamin either. In fact, it acts more like testosterone or cortisol than a nutrient you get from food. The only reason we still call it a vitamin is because scientists misclassified it a century ago, and the name stuck.
The mechanism behind vitamin D in the body is surprisingly complex. When UV-B light (from sun light) hits your skin, it reacts with a cholesterol compound called 7-dehydrocholesterol, producing vitamin D₃ (cholecalciferol) — the same molecule you’ll find in most supplements.
From there, the liver converts it into calcifediol (25-hydroxy-vitamin D), which is the storage form measured in blood tests. Finally, your kidneys (and even some immune cells) turn that into calcitriol, the active hormone that flips genetic switches throughout your body.
So when you take a vitamin D₃ capsule, you’re not taking the finished product — you’re just sending the raw material into the system. Whether it ever becomes the active hormone depends on how well your liver and kidneys are working, and whether you have enough magnesium, vitamin K₂, and vitamin A to support those conversions.
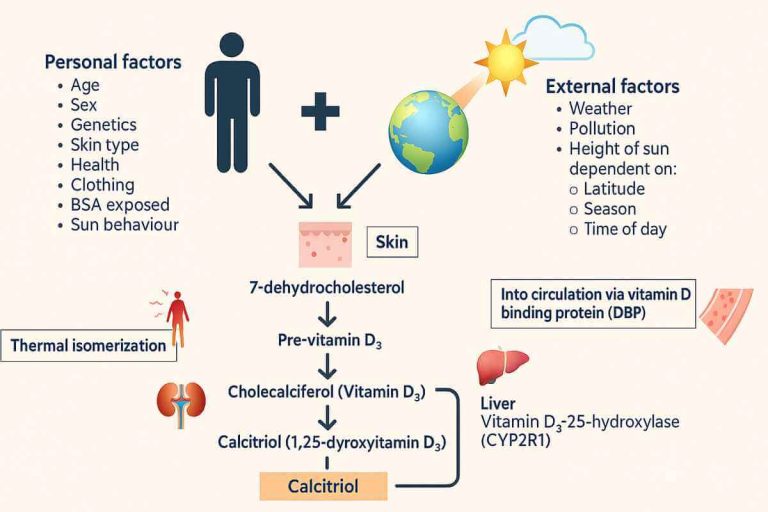
Whether vitamin D₃ comes from sunlight, food, or a supplement, the molecule itself is the same — cholecalciferol. What matters isn’t where it comes from, but what your body does with it. Every source feeds into the same pathway: first the liver, then the kidneys, then your cells.
But how efficiently you process it depends on your biology — your liver health, magnesium and K₂ levels, and even how inflamed or metabolically healthy you are. In other words, the pill and the sun give you the same raw material, but not always the same result.
The Real Role of Vitamin D in Health
Once vitamin D is converted into its active form — calcitriol — it stops acting like a nutrient and starts behaving like a master regulator. Calcitriol binds to receptors inside your cells and directly influences the expression of hundreds of genes, touching nearly every system in the body.
Its most obvious job is in calcium and bone metabolism — helping your gut absorb calcium, keeping it in your bones, and preventing it from floating around in your bloodstream. But that’s only part of the story.
Vitamin D also plays a major role in immune regulation, helping your body strike the balance between defense and inflammation. It ramps up the production of antimicrobial peptides that fight off bacteria and viruses, while keeping your immune system from going into overdrive and attacking your own tissues.
Beyond immunity, vitamin D is deeply tied to hormone balance, mood, and metabolic health. Low levels are linked with insulin resistance, low testosterone, depression, fatigue, and a sluggish metabolism. It doesn’t mean vitamin D cures those conditions — but it’s often the silent foundation beneath them.

Vitamin D and the Immune System
What makes vitamin D so essential to health goes far beyond its role in bone strength — it’s one of the cornerstones of your immune defense. When a cold or flu hits, most people reach for vitamin C, but it’s often vitamin D quietly working behind the scenes that determines how well your immune system holds the line. As long as your levels aren’t running low (which many people are), vitamin D is one of the body’s most effective natural defenses.
When your immune cells detect a threat, they don’t just react blindly; they actually convert vitamin D’s storage form (calcifediol) into its active hormone, calcitriol, right inside the cell. That hormone then switches on genes that make powerful antimicrobial peptides like cathelicidin and defensins — natural antibiotics your body manufactures to destroy bacteria, viruses, and fungi before they spread.
Vitamin D also keeps the immune system from going rogue. It tones down excessive inflammation by regulating cytokine production, helping your body fight what’s dangerous without turning on itself.
This “immune intelligence” is one reason vitamin D sufficiency is linked to lower rates of respiratory infections, fewer autoimmune flares, and a more balanced inflammatory response overall.
But none of this works if your fuel tank (calcifediol) is empty. The immune system draws on circulating vitamin D reserves when infection strikes. If those levels are low, your cells can’t make enough active hormone fast enough to mount an effective defense.
Studies have shown that people with adequate vitamin D status tend to get fewer and less severe infections, while late supplementation (especially large one-time doses) often shows little benefit — simply because the timing is too late for the biology to catch up.
Think of vitamin D not as an emergency medicine, but as preventive architecture. You build the structure long before you need it. Keeping your vitamin D levels topped up is like keeping your immune weapons loaded — not to use all the time, but to make sure they’re ready when the fight comes.
Why Timing Matters: Vitamin D Takes Time to Work
Here’s the catch with vitamin D that most miss — it isn’t an instant shield. The D₃ molecule itself does almost nothing until your body processes it through several slow, biological steps.
When you ingest vitamin D, whether through food or through supplementation, it first has to pass through your liver, where enzymes convert it into calcifediol (the storage form measured in blood tests). That conversion alone can take a week or two, depending on your metabolism, magnesium levels, and overall liver health. Only after that does your kidney and immune tissue transform it into calcitriol, the active hormone that actually empowers your immune cells.
That means taking vitamin D₃ when you’re already sick is often too late to make a difference. You can’t flood your system overnight and expect your immune army to be ready by morning. The real protection comes from consistency — keeping your vitamin D stores topped up long before infection strikes.
For those living in colder or less sunny climates, keeping your vitamin D “fuel tank” topped up is even more critical. The form that actually circulates in your blood — calcifediol [25(OH)D] — acts as your body’s reserve supply, ready to be activated when needed.
Studies show that infections peak during winter, precisely when calcifediol levels are at their lowest. Since it takes weeks for vitamin D₃ to convert into this usable form, the time to prepare isn’t when you get sick — it’s a month or two before winter, by increasing sunlight exposure or slightly raising your vitamin D intake ahead of time.
The same principle applies to sunlight, though with a gentler curve. When your skin makes vitamin D₃ from UV-B light, that raw D₃ still travels the same path: skin → liver → calcifediol → calcitriol. The difference is that sunlight gives you smaller, steadier doses that your body can process naturally over time, avoiding the spikes and delays that come with large supplement doses.
It’s important to remember that Vitamin D isn’t an emergency response — it’s a standing defense system. You don’t build it when you’re under attack; you build it beforehand, through regular sunlight, nutrient support, or smart supplementation that keeps your “fuel tank” full year-round.
What are the Main Forms of Vitamin D?
There are three ways to get vitamin D: sunlight, food, and supplements. Only one of them is truly natural — the sun — and the other two exist because we drifted too far from it.
Sunlight — The Preferred Source
For most of human history, we lived outdoors — hunting, gathering, building, walking, and sleeping under open skies. Our skin made vitamin D₃ daily, naturally, and in balance. The process was self-regulating: sunlight triggered production, but too much UV-B destroyed any excess before it entered the bloodstream. You couldn’t overdose, and you didn’t need to worry about cofactors — the body handled it perfectly.
Food — The Top-Up System
In parts of the world where sunlight was scarce, nature provided a Plan B. Traditional northern diets were rich in vitamin D–dense foods — oily fish, cod liver, egg yolks, wild game, animal fats, and organ meats. Indigenous populations in the Arctic, for instance, stayed healthy through long, sunless winters because their diets were packed with vitamin D and its cofactors like vitamin A and omega-3 fats. It wasn’t the climate that protected them — it was the food ecosystem that evolved alongside it.
Supplements — The Backup System
Supplements are the third and newest source — a synthetic stand-in for the sunlight and diets most of us have lost. They’re incredibly useful, especially if you live in high latitudes, work indoors, or rarely see the sun. But they’re not a perfect substitute.
Supplements deliver the raw material (cholecalciferol), but not the context — no light cues, no circadian benefits, and no built-in self-regulation. And unlike natural sources, they can unbalance calcium metabolism if you’re low in magnesium or vitamin K₂, nutrients that used to come bundled in ancestral diets.
Evolution didn’t make a mistake by misjudging our vitamin D needs. Humans were perfectly adapted to make and store vitamin D through regular sun exposure and nutrient-rich foods. The “deficiency epidemic” only began when we built lives that cut us off from both, such as working in an office all day or avoiding meats and animal fats. Supplements exist not because nature failed, but because we stopped living in nature’s design.

Why Deficiency Is So Common
If vitamin D is so essential, why are so many of us still running on empty? Geography, skin tone, diet, and lifestyle all play a part. Above about 37° latitude, winter sunlight is too weak to trigger vitamin D production at all.
People with darker skin need much more sun exposure to make the same amount, putting them at greater risk in northern climates. Add to that modern diets low in seafood and animal fats, aging skin that produces less 7-dehydrocholesterol, and body fat that traps vitamin D, and it’s easy to see why deficiency has become the rule, not the exception. The body hasn’t failed — the environment has changed.
Sunlight vs Supplements — What’s the Difference?
Vitamin D₃ from sunlight and vitamin D₃ from a supplement are chemically identical, but how your body handles them couldn’t be more different. One is made through a tightly regulated natural process; the other bypasses that system entirely.
When UV-B light hits your skin, it converts a cholesterol compound (7-dehydrocholesterol) into vitamin D₃ right inside your epidermis. The process has a built-in off-switch: once you’ve made enough, continued UV-B exposure actually destroys the extra D₃ before it enters your bloodstream. That means you can’t “overdose” on sunshine — your body automatically keeps levels in check.
Supplements, on the other hand, deliver a fixed, unregulated dose directly into your system. There’s no feedback loop to stop absorption, so chronic high intake can raise blood levels far beyond what nature ever intended. That’s why supplementing blindly, without testing, can lead to problems with calcium regulation and soft-tissue calcification — especially if you’re low in magnesium or vitamin K₂, the nutrients that keep calcium in bone where it belongs.
There’s also the matter of what comes with sunlight. Natural light triggers nitric oxide release, resets circadian rhythms, boosts serotonin, and improves mitochondrial function — benefits you don’t get from a pill. Sunlight is a biological signal, not just a source of vitamin D.
Supplements still have their place — particularly for people in dark winters, high latitudes, or jobs that keep them indoors. But the goal should always be to mimic nature, not replace it: modest, consistent doses that maintain healthy blood levels, rather than large, irregular hits that we need to balance manually.
Vitamin D Toxicity – Can you Supplement Too Much?
Like most things in biology, vitamin D follows a bell curve — too little, and your system struggles; too much, and the very thing meant to heal you can start to harm.
Vitamin D toxicity is rare, but it happens when supplement intake consistently exceeds what the body can regulate. Typically, scientific literature caps this limit at around 5000IUs per day,or 10,000 IU per day for around a month maximum.
More recent research, however, has found no ill effects from long-term use of up to 10,000 IU per day. For example, a multi-year study in a psychiatric hospital in Ohio reported that patients taking either 5,000 or 10,000 IU of vitamin D₃ daily for over a year — some for several years — showed no signs of toxicity or hypercalcemia, with average blood levels rising safely to between 68 and 96 ng/mL.
While more modern literature finds higher dosages of up to 10,000 IU per day safe long-term, the mixed results leaves an element of doubt, something which can be avoided altogether by obtaining vitamin D from sunshine and food.
The problem isn’t the vitamin D molecule itself — it’s what it does downstream. Active vitamin D (calcitriol) increases calcium absorption from the gut. When you flood your system with D without balancing nutrients like vitamin K₂ and magnesium, that calcium doesn’t all end up in your bones — it starts circulating in your bloodstream, where it can calcify soft tissues, harden arteries, and stress the kidneys.
There lies a great difficulty here in knowing what the balance is in your body. You may have enough vitamin K2 and Magnesium in your body already. Or you may be deficient, depending on variables including genetics and your diet.
Interestingly, some studies have experimented with very high, short-term doses of vitamin D₃ — in the hundreds of thousands of IU — to fight chronic or severe infections, with some preliminary success.
A 2025 study from Semmelweis University found that hospitalized COVID-19 patients who received a short, moderately high-dose regimen of vitamin D₃ (three doses of 30,000 IU, totaling 90,000 IU) saw a 67% reduction in mortality, without any cases of toxicity or abnormal blood levels.
Within just four days, their vitamin D deficiency was fully corrected, and both calcifediol and calcitriol stayed within normal ranges. This shows that when deficiency is corrected quickly and safely, the body can better mount its immune defenses — and that toxicity concerns around well-structured high-dose supplementation may be overstated.
Nature has already built the perfect safeguard: sunlight. When you get vitamin D from the sun, there’s no risk of overdose. The same UV-B rays that create vitamin D also destroy the excess, keeping your levels perfectly balanced. Supplements don’t have that self-regulating mechanism, which is why restraint and co-nutrients matter.
It’s also worth noting the confusion that arose during the COVID pandemic. Early studies testing vitamin D₃ supplementation found no measurable benefit, but most of those trials only lasted a few days. We now understand why: taking cholecalciferol (D₃) only starts the process — it still needs to be converted by the liver into calcifediol, and then by the kidneys or immune cells into calcitriol, the active hormone that supports immune defense.
That conversion can take weeks, by which time an acute infection has already run its course. Later research using the active form (calcitriol) or pre-hydroxylated calcifediol directly showed more promising results, supporting the idea that maintaining healthy vitamin D stores before infection — not during it — is what truly makes the difference.
In short, vitamin D doesn’t work alone, and it doesn’t work instantly. It’s part of a tightly choreographed system that depends on sunlight, co-nutrients, and time. Treat it with respect, and it rewards you with balance. Abuse it, and you lose the very harmony it’s meant to create.
Not All Sunlight Is Equal — The Variables That Matter
You can stand next to someone in the same sunshine and walk away with totally different amounts of vitamin D. That’s because sunlight isn’t a fixed dose — it’s a constantly shifting mix of geography, season, and biology.
The biggest factor is latitude. Above about 37 degrees north or south, the sun sits too low in the sky during winter for its UV-B rays to reach the ground in strength. You could sunbathe all day in London or Toronto in January and still make almost no vitamin D. Closer to the equator, UV-B remains strong year-round, which is why traditional equatorial diets and darker skin evolved as protective balances rather than compensations.
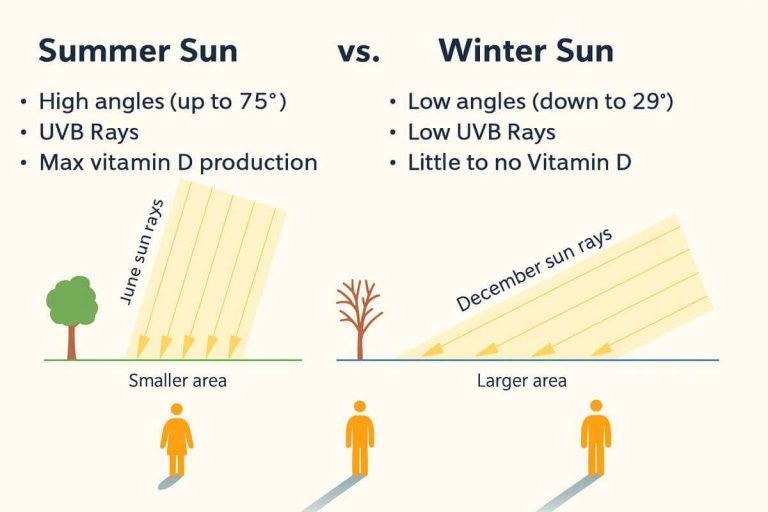
Season and time of day matter just as much. Vitamin D synthesis peaks when the sun is high — roughly between 10 a.m. and 2 p.m. Morning and late-afternoon light is rich in UV-A (the kind that tans and ages the skin) but low in UV-B, which is the only wavelength that triggers vitamin D production.
Then there’s skin tone. Melanin acts like natural sunscreen: the darker your skin, the longer you need in the sun to make the same amount of vitamin D as someone with lighter skin. That’s protective in the tropics, but it makes deficiency far more common for darker-skinned people living in northern climates.
Cloud cover, pollution, altitude, and surface area all add to the equation. Thick clouds or smog can block most UV-B. Higher altitudes, where the air is thinner, increase it. And the more skin you expose, the more vitamin D you make — ten minutes in a T-shirt isn’t the same as ten minutes in a bathing suit.
Even age plays a role: older skin contains less 7-dehydrocholesterol, the raw material used to create vitamin D₃, meaning production naturally slows with time.
So “getting some sun” isn’t a one-size-fits-all prescription. It’s a moving target shaped by who you are, where you live, and how you live. The key is finding your own sweet spot — enough sunlight to keep your biology humming, but not enough to burn.
The Case For Supplementation
If sunlight is nature’s plan A, and food is plan B, then supplements should form plan C. They exist because we’ve built lives that cut us off from the natural rhythms our bodies evolved for.
In a perfect world, most people wouldn’t need a vitamin D supplement at all. Daily exposure to the sun and nutrient-rich foods like fatty fish, cod liver, egg yolks, and organ meats would easily keep levels in a healthy range.
But that’s not how most of us live anymore. We wake before sunrise, work indoors, drive instead of walk, and step into the sun only long enough to move from one shaded spot to another. Add long winters, pollution, sunscreen (see here for the hidden dangers of sunscreen), and darker skin tones in low-UV environments — and deficiency becomes almost inevitable.
That’s where supplementation earns its place — not as a shortcut, but as a backup system. A vitamin D₃ capsule gives you the same molecule your skin makes from sunlight — it just skips the UV-B step. The problem is, that UV-B step is also what keeps nature in balance.
When vitamin D is made in your skin, excess is automatically broken down by the same sunlight that created it. With supplements, that self-regulating mechanism is gone, so you have to provide the regulation yourself — by dosing wisely and staying aware.
Testing your vitamin D levels technically requires a blood test — specifically the 25-hydroxyvitamin D [25(OH)D] test — and while that’s ideal, it’s not always practical. A healthy range is generally around 40–60 ng/mL (100–150 nmol/L) (some recommend 20 ng/mL but this is for bone health, not immune function). To summarize, the “bone-health” dosage (600–800 IU/day) keeps you from disease while the “immune-health” dosage (2,000–5,000 IU/day) keeps you at your biological best.
If testing isn’t an option, you can still estimate from lifestyle and environment: people who spend most of their time indoors, live far from the equator, go through long winters, or have darker skin in low-UV climates are much more likely to be deficient. In those cases, a modest daily supplement through the winter is a safe insurance policy. If you regularly get midday sun on bare skin for 15–30 minutes a few times per week, you’re probably maintaining healthy levels naturally.
And remember, vitamin D doesn’t work alone. It needs magnesium to activate the enzymes that convert it, and vitamin K₂ to make sure the extra calcium it helps absorb ends up in your bones — not your arteries. Ignoring those cofactors is how supplementation goes from helpful to harmful.
So think of vitamin D supplements as the final tier in the hierarchy:
- Sunlight first — the natural, self-regulating source.
- Food second — the nutrient-rich backup nature intended.
- Supplements third — the modern patch when life, latitude, or lifestyle make the first two impossible.
Used this way — as a bridge, not a crutch — supplementation isn’t a flaw in evolution; it’s a way to correct a flaw in how we live.
The Case Against Supplementation
For all its benefits, vitamin D is one of the most misunderstood and overused supplements in modern health. The issue isn’t the molecule — it’s the mindset. We’ve been conditioned to believe that if something is good, more must be better. But biology doesn’t work that way.
When you take vitamin D₃, you’re sending a chemical signal into a complex hormonal system. If that system isn’t supported by the right cofactors — like magnesium, vitamin K₂, and vitamin A — the extra vitamin D can start moving calcium to the wrong places. Instead of strengthening bones, it can harden arteries, strain kidneys, and calcify soft tissues over time. The danger isn’t immediate, which makes it even more deceptive. You’ll feel fine right up until you’re not. While reports of this are rare, it’s not impossible.
Another problem is that many people supplement without need or context. They never test their levels, they take megadoses “just in case,” or they chase internet anecdotes claiming that more vitamin D will fix everything from fatigue to depression. Meanwhile, most studies show that once you’ve reached healthy blood levels (around 40–60 ng/mL), taking more does nothing extra — and can, in some cases, tip the scales toward harm.
Even the timing matters. Supplementing after you get sick won’t suddenly boost your immunity — the conversion from cholecalciferol (vitamin D₃) to its active hormone can take weeks. By that point, the infection has already run its course. The real benefit comes from maintaining good levels consistently, not reacting when symptoms appear.
So the argument isn’t against vitamin D — it’s against treating it like a quick-fix pill. Supplements are useful, but they work best when they’re earned by need, not habit. In an ideal world, sunlight and diet should be enough. If they’re not, use supplements intelligently — as a measured tool, not a daily crutch.
Practical Takeaways
You don’t need to memorize the biochemistry to use vitamin D wisely — just remember how nature designed it and how to work with that design, not against it.
- Sunlight first. Aim for short, regular sun exposure on bare skin, ideally midday, when UV-B is strongest. Ten to twenty minutes, a few times a week, is enough for most light-skinned people. Darker skin needs longer — sometimes two to three times more. The goal is to get light, not a burn.
- Food second. Eat foods that naturally contain vitamin D: salmon, sardines, cod liver, egg yolks, liver, and grass-fed butter. These also come packaged with vitamins A, K₂, and omega-3 fats, the natural cofactors that keep the system balanced.
- Supplements third. Treat supplements as a modern backup plan, not a daily default. If you can’t get enough sunlight or vitamin D–rich foods, take 1,000–2,000 IU per day as a modest, consistent dose — or more under guidance if you’re deficient. Always combine with magnesium and vitamin K₂ to keep calcium in check.
- Test when possible. The best way to know where you stand is with a 25-hydroxyvitamin D [25(OH)D] blood test. A healthy range is 40–60 ng/mL (100–150 nmol/L). If you can’t test, assume deficiency is likely if you live far from the equator, work indoors, or have darker skin in a low-sun climate.
- Avoid extremes. Mega-dosing vitamin D “just in case” can backfire. More isn’t better; balance is. The goal is to maintain steady levels, not chase high ones.
- Remember the bigger picture. Sunlight provides far more than vitamin D — it anchors your circadian rhythm, supports mental health, and improves metabolic function. Supplements can’t replicate that.

As with most things, live closer to how you were designed. Get light. Eat real food. Supplement only when needed. Nature has provided everything you need, so learn to live alongside it, not against it.
FAQs
What does vitamin D do for your body?
Its most obvious job is in calcium and bone metabolism — helping your gut absorb calcium, keeping it in your bones, and preventing it from floating around in your bloodstream. But that’s only part of the story.
Vitamin D also plays a major role in immune regulation, helping your body strike the balance between defense and inflammation. It ramps up the production of antimicrobial peptides that fight off bacteria and viruses, while keeping your immune system from going into overdrive and attacking your own tissues.
How long do you need to be in the sun to get vitamin D?
If you regularly get midday sun on bare skin for 15–30 minutes a few times per week, you’re probably maintaining healthy levels naturally.
How much vitamin D should you take daily?
Treat supplements as a modern backup plan, not a daily default. If you can’t get enough sunlight or vitamin D–rich foods, take 1,000–2,000 IU per day as a modest, consistent dose — or more under guidance if you’re deficient. Always combine with magnesium and vitamin K₂ to keep calcium in check.